Osteoporosis Screening: What You Need to Know
Amy Barczy
| 4 min read
Amy Barczy is a former brand journalist who authored content at Blue Cross Blue Shield of Michigan. Prior to her time at Blue Cross from 2019-2024, she was a statewide news reporter for MLive.com. She has a decade of storytelling experience in local news media markets including Lansing, Grand Rapids, Holland, Ann Arbor and Port Huron.
Screening for osteoporosis is an important part of regular health visits for women and men, especially once they reach a certain age. Often, the signs and symptoms of osteoporosis occur when the disease has progressed to the point that someone fractures or breaks a bone. This is why it’s important to visit a health care provider for an annual physical to ensure you stay on top of your health and stay on track with needed screening tests.
What causes osteoporosis?
Osteoporosis is a common disease that causes bones to become brittle and weak such that a simple fall or minor stress can cause a fracture.Osteoporosis does not equally affect the bones. The most affected bones are the spine, the hips and the wrists. Collapse of the spine is especially significant since it can cause a significant loss of height, sometimes up to six inches, and a stooped forward posture.
There are risk factors, including age, a sedentary lifestyle, family history, cigarette use, early menopause in women, long-term use of steroids or immunosuppressants, low testosterone in men, certain medical conditions and thyroid disease.
Men, in general, because of their greater size, have stronger, denser bones than women and a lower risk for osteoporosis. African Americans generally have stronger, denser bones than Caucasian individuals and are at a lower risk for osteoporosis. Women who have smaller frames, are of older age and of Asian heritage are at the highest risk for osteoporosis.
What is an osteoporosis screening?
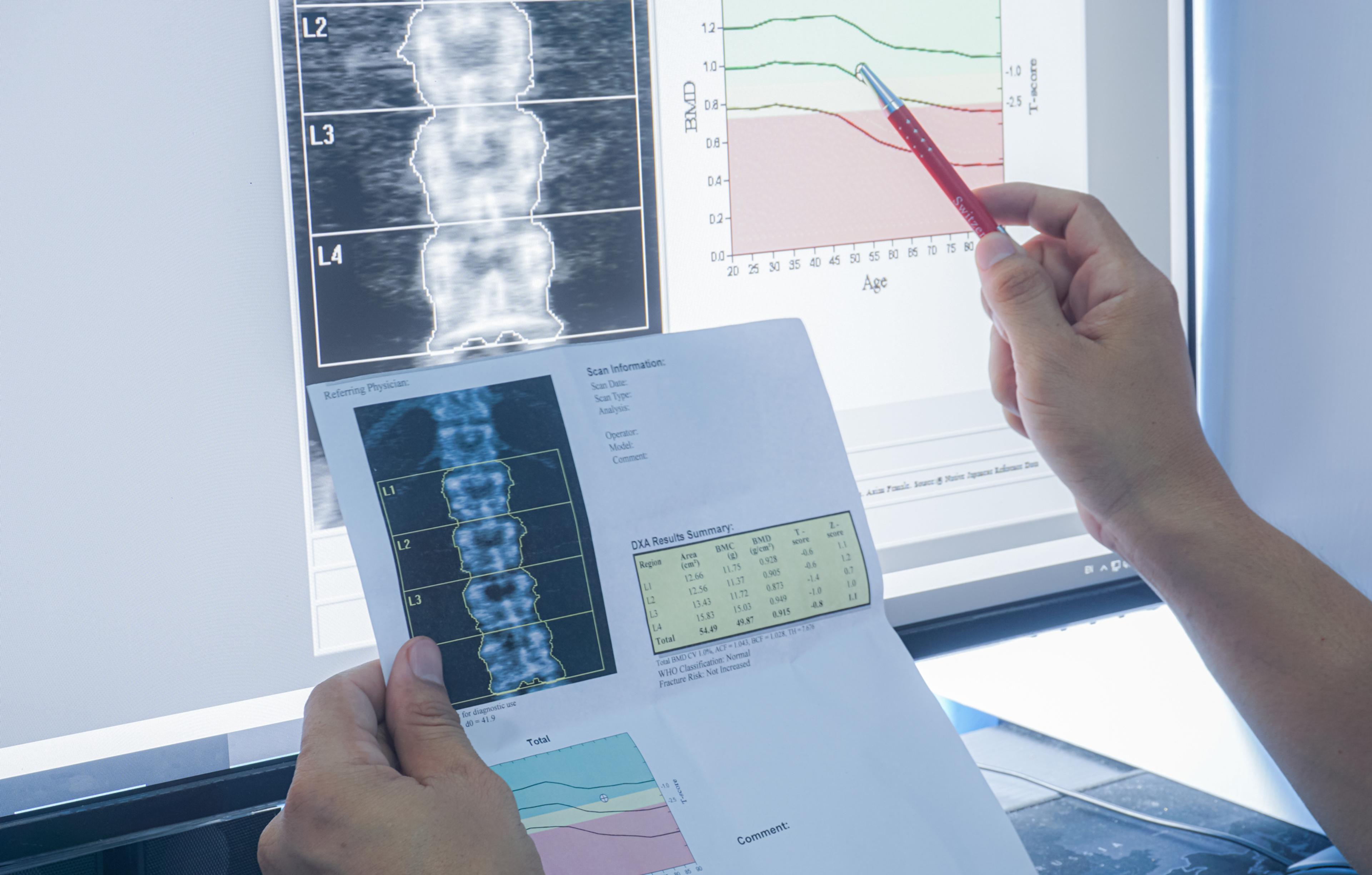
Health care providers use a bone density test to screen for osteoporosis. This is a test that uses X-rays to determine how many grams of calcium and other minerals are in a segment of bone. The higher the bone mineral content, the denser bones and stronger bones are.
The tests are typically done on the bones that are most likely to break, including the lower spine, the top of the thighbone next to the hip joint and bones in the forearm.
When conducted early enough, bone density tests are an effective way to monitor any decreases in bone density to allow for an early diagnosis. This allows for simple, effective treatments that can help prevent fractures, deformities and other complications that come with advanced osteoporosis.
When do I need an osteoporosis screening?
Health care providers will likely begin discussing risk factors for osteoporosis with you if they think you need to be screened for osteoporosis. Otherwise, women should be screened with a bone density test beginning at age 65.
What happens after an osteoporosis screening?
Your health care provider can help you interpret the results of a bone density test to determine if your bone density is considered normal, below normal or low enough to indicate you likely have osteoporosis.
If your bone density test does not return a normal result, your health care provider will likely make treatment recommendations that could include diet and lifestyle changes, medication and surgery.
What are the symptoms of osteoporosis?
Since osteoporosis develops slowly over years it may not be noticed until there is a fracture. Loss of height can be an indicator because of the collapse of the spine. Wrist and hip fractures may also indicate osteoporosis.
Because the risk of osteoporosis is affected by factors including race, sex, age, height, diet and behavior, individuals need to have a sense of their own risk and discuss it with their primary care provider. Physicians can make recommendations that include diet, exercise, screening tests such as bone densitometry, calcium and vitamin D supplements and prescription medications, if needed.
How do I prevent osteoporosis?
Bone strength and density depends upon nutrition and exercise. It’s important to follow these best practices at every age to keep the body strong and healthy:
- The body needs calcium and vitamin D for healthy bones.
- Food sources of calcium include dairy products, vegetables with dark green leaves, canned salmon, sardines with bones, soy products like tofu, calcium-fortified foods and cereals.
- The most natural source of vitamin D is exposure to sunlight. However, in northern climates such as we have in Michigan, with cloud cover and colder weather, vitamin D supplements may be needed. Most food has very little vitamin D unless it is specifically fortified, such as milk or certain brands of orange juice. Oily fish, egg yolks and mushrooms contain small amounts of vitamin D.
- Exercise is important but should be weight bearing and not low impact to stimulate bone strength and density. Talk to your doctor before beginning any new exercise routine.
- Weight-bearing exercise is important for bone health, including walking, jogging, running, stair climbing and skiing. This type of exercise helps the hips, legs and lower back.
- Strength training is also important to ensure muscles and bones in the upper back and arms stay healthy.
- Limiting substance use.
- Limiting the risk for falls is especially important for older adults.
Learn more about how preventive care can help you live a healthier life here on MIBluesPerspectives.com.
Photo credit: Getty Images





