Integrating Mental Health Care into Primary Care Can Lead to Better Outcomes
Julie Bitely
| 4 min read

If you’re struggling with diabetes, but also suffer from depression, making sure you’ve checked your blood sugar and taken your insulin might not be a top priority. Treating patients with both medical and mental health issues was the topic of the most recent monthly Health Forum of West Michigan, sponsored by Blue Cross Blue Shield of Michigan. A panel of experts agreed that integrating mental health care into routine medical treatment shows promise. Not only will an integrated approach potentially catch more people struggling with anxiety and depression, but it’s proven to be a cost-effective way to control and improve acute medical conditions. So, what exactly is integrated care? Phil Baty is a family physician and medical director at Mercy Health Physician Partners. He and other panelists pointed to a program called COMPASS (Care of Mental, Physical and Substance Use Syndromes), a care management model designed to improve the care of patients with depression and diabetes and/or cardiovascular disease, and hypertension. The COMPASS model consists of a team of providers, nurse care managers, other members of the primary care practice team, and support services to follow patients with complex care needs. Baty had been treating a patient with diabetes for years. After his wife died, the patient also struggled with severe depression. As his doctor, Baty was primarily treating the diabetes, but the depression was holding the patient back. When Baty’s practice adopted the COMPASS model, which introduced care managers into the primary care setting, this particular patient took part. He eventually was able to get his blood pressure under control, his markers for diabetes went down and his depression improved. “This program has put him back into the life he once knew,” Baty said. Doctors like Baty, who are primarily trained to deal with the medical issues a patient presents with, are able to transfer patients to care managers. The care managers are able to spend more time with patients and can then connect them to other services if necessary. Kiran Taylor is the division chief of psychiatry and behavioral medicine at Spectrum Health Medical Group. She said as a provider, Spectrum is working to be proactive by implementing their Psychiatry Behavioral Model (PBM+) in primary care settings, another integrated approach to care. Whereas old ways of treating mental illness and medical conditions are fragmented and operate in silos, Kiran said PBM+ ensures that everyone has an initial mental health screening. If necessary, patients are then moved on to an integrated behavioral health specialist who can recommend specific interventions based on the severity of patient need. Kiran said screenings could expand to other areas of care such as neurology and oncology. She pointed out that integrated screenings and treatment helps patients who might not even realize they’re struggling with mental illness or who would otherwise be reluctant to admit it for fear of stigma. Out-of-the-box thinking is needed in Michigan, which ranks 41st out of 50 states and Puerto Rico in terms of having a high prevalence of mental illness and low access to care. Kiran said integrated care provides the best of both worlds in that it improves quality of care while driving down costs.
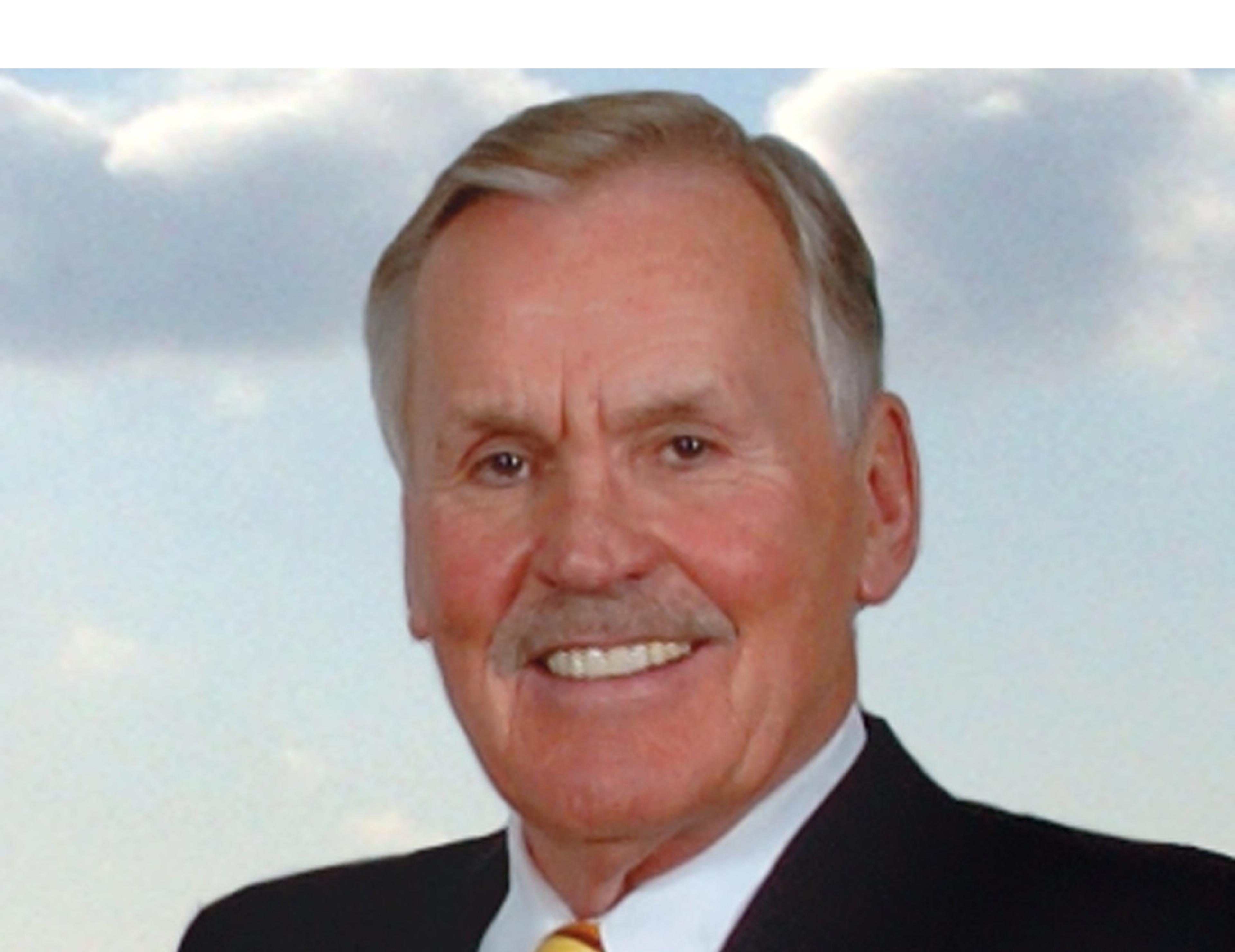
Dr. William Beecroft Blue Care Network medical director of behavioral health William Beecroft said insurers, including Blue Cross, are looking to be innovative when it comes to paying for integrated approaches because they are so effective. He said for a patient with three chronic illnesses such as diabetes, hypertension, and COPD as well as depression, treatment can cost about $60,000 per year. However, if you treat the depression to remission, costs will be closer to $12,000 per year with improved outcomes. “The improvement in quality of life for the member is a main benefit,” Beecroft said. If you’re interested in future Health Forum of West Michigan events, visit their website to register. May’s panel will continue the conversation about integrating mental and behavioral health with physical medicine. All events are free and open to the public. If you enjoyed this post, you might also like: