‘We’re Finally Talking About It’: Panelists Address Mental Health
Julie Bitely
| 3 min read
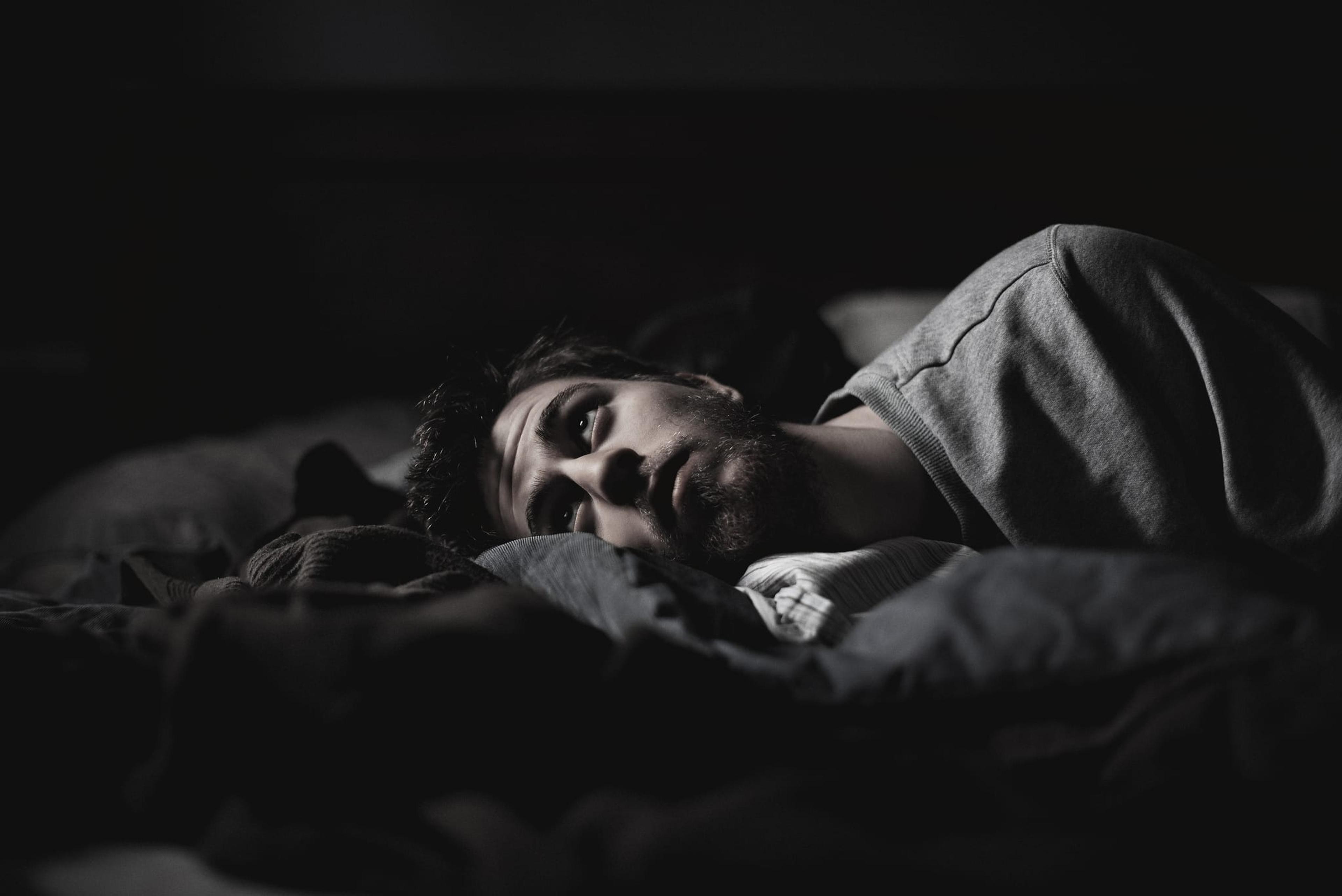
Would it surprise you to learn that depression reduces life expectancy as much as smoking or that more people die every year by suicide than they do in car accidents? Mental health is a complex topic with many different players attempting to address it. A panel of experts took up the issue at the most recent Health Forum of West Michigan, where community conversations are held the first Friday of every month at Grand Valley State University. Blue Cross Blue Shield of Michigan and Blue Care Network sponsor the events. With 25 percent of Americans suffering from mental illness and nearly 50 percent of U.S. adults expected to develop at least one mental illness during their lifetime, it’s a conversation that needs to happen, panelists said. “We’re finally talking about it as a country,” said Mark Eastburg, Chief Executive Officer and President, Pine Rest Christian Mental Health. The most common diagnoses are anxiety and depression. Eastburg said any mental illness has the potential to not only disrupt the affected individual, but cause a ripple effect on family members and employers. Loved ones of a person with a mental illness have a “family ache”, Eastburg explained, while he pointed out that 40 percent of all sick days are related to mental illness. Additionally, depression and anxiety are two of the top five conditions driving health care spending and care for mental health and substance abuse disorders is two to three times more costly. At an individual level, people with serious and persistent mental illness die 25 years younger than the general population and those with depression are 50 percent more likely to develop heart disease, stroke, lung disease, asthma and arthritis. “These are risky diseases,” Eastburg said. “These have an impact on mortality.” Ensuring access to treatment needs to be a community-wide, collaborative effort, panelists agreed. “We’ve got a crisis of access in our country today,” Eastburg said. Scott Gilman is the Chief Executive Officer at Network 180, the community mental health authority for Kent County. The agency is responsible for ensuring that county residents with serious and persistent mental illness, intellectual or developmental disabilities and substance use disorders are able to access care. Earlier this year, some services had to be cut as a result of budget shortfalls. Gilman said innovation is needed to reach the most vulnerable members of society so that they can get the help they need. David Blair, MD, is President and Chief Medical Officer at Mercy Health Physician Partners. He said the health system is working to innovate in the mental and behavioral health space through efforts that focus on social determinants of health, establishing best practices around prescribing opioids and expanding clinics in underserved parts of the community. At Pine Rest, Eastburg said the organization is trying to address psychiatric wait times by focusing on a residency program that will hopefully establish a broader workforce in West Michigan. Pine Rest also works to expand access by partnering with primary care clinics and hospitals and offering services to schools, churches and businesses. “We have to reach out to people where they are,” he said. Learn more about the Health Forum of West Michigan. If you enjoyed this post, you might also like:
- Panic Attacks: What to Do If They Happen at Work
- Mental Health on the Job: Tips for Ending Stigma at Work
- Combatting a Hidden Health Crisis: Chronic Stress
Photo credit: Ansel Edwards





