University of Michigan Peer-Delivered Oral Health Intervention Educates and Facilitate Dental Care to People with Psychiatric Disabilities

Jake Newby
| 5 min read
Jake Newby is a brand journalist for Blue Cross Blue Shield of Michigan.

When the connection between physical and mental health is discussed, oral health’s role in that relationship is often understated. But it shouldn’t be.
Two University of Michigan researchers launched a peer-delivered oral health intervention for individuals with psychiatric disabilities. The goal of the project was to train community health workers, peer support specialists and peer recovery coaches to understand the problem of oral health issues among those with psychiatric disabilities, so they could provide oral health education and help facilitate dental care.
“We know that people with severe and persistent mental illnesses are more than three times likelier to lose their teeth than those who aren’t,” said Dr. Danielle Rulli, a University of Michigan School of Dentistry faculty member and dental hygienist.
Dr. Rulli and Dr. Adrienne Lapidos – a clinical associate professor in the department of psychiatry at the U of M Medical School – received funding from the Blue Cross Blue Shield of Michigan (BCBSM) Foundation in 2022 to help them launch the latest phases of their ongoing project. The $55,000 Investigator Initiated Research Award has allowed Lapidos, Rulli and their team to conduct research and training.
“Dr. Rulli and I worked with a community advisory board of individuals who work in these settings – or have a lived experience themselves of receiving treatment in these settings – and to think together about how we can raise awareness about oral health in behavioral health settings” Lapidos said. “How do we promote oral wellness without needing to have a dentist or dental hygienist on site to provide that information.”
It wasn’t an objective to certify new dentists. The training was meant to equip lay care health workers with the tools and knowledge needed to have appropriate conversations with people in these vulnerable populations about oral health; to have frank discussion about the shame and stigma sometimes associated with oral health problems.
“We want them to be that link, to be that bridge to the dental team,” Lapidos said. “To help that person in need make an appointment if fear or other barriers have prevented that appointment from being made.”
The bidirectional relationship between oral health and behavioral health
In health, a bidirectional relationship occurs when one issue enhances or exacerbates another, and vice versa. In this instance, mental health and oral health have a bidirectional relationship.
“There are very important ways that oral health impacts mental health and systemic health, but it goes in the other direction, as well,” Lapidos said. “Mental health and substance use disorders impact oral health … Mental health diagnoses often come along with problems with energy and motivation and that impacts people’s ability to care for their oral health.”
Medications that people take for mental health diagnoses often cause dry mouth or xerostomia, Lapidos said, which are major risk factors for developing oral diseases. Additionally, illicit substance used as part of a substance use disorder can cause tooth decay.
“What all of this tells us is the relationship between oral health and behavioral health is bidirectional” Lapidos said.
‘People-centric, not provider-centric:’ Results yielded by the project
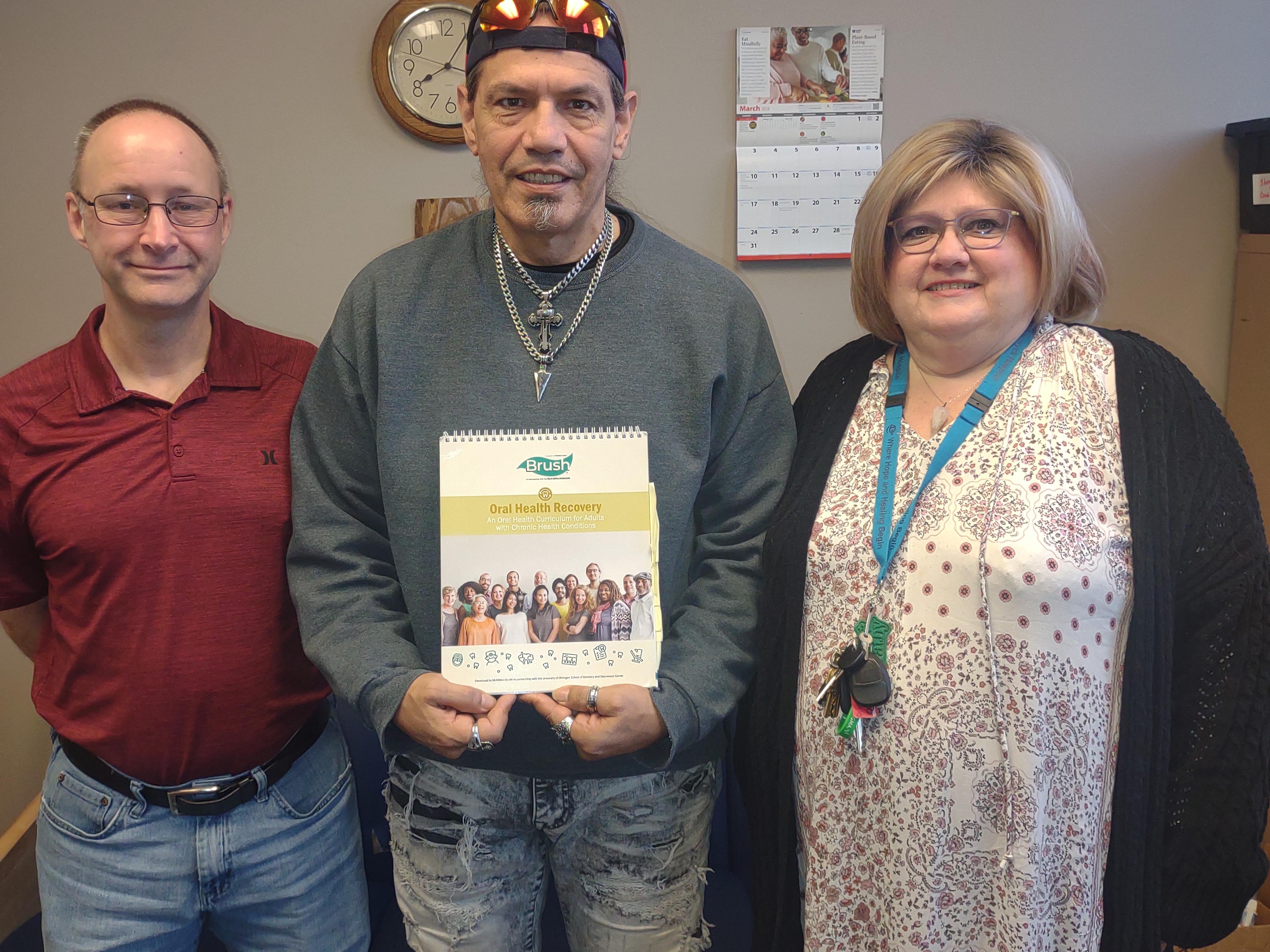
Prior to BCBSM’s involvement and during the previous stage of this project, the U of M researchers developed a flip chart that essentially served as a teaching tool. It allowed people with psychiatric disabilities to facilitate oral health discussions and increase motivation to seek dental care.
“The things they prioritized were different than what we’d assume,” Dr. Rulli said. “For example, they said, ‘We know we should stop smoking, don’t talk to us about quitting smoking; talk to us about how that impacts my gums and my teeth.’ And that was very eye-opening for me. That was very people-centric, not provider-centric.”

Dr. Lapidos and Dr. Rulli found that within about two months, over half the people with psychiatric disabilities reported that they had met a dental self-care goal because of the program.
“We also found that 27% in our oral health recovery group and 36% in our video comparison group reported that they made a dentist appointment because of the program,” Dr. Lapidos said.
“This research project demonstrates the power of collaboration and integrated health care,” said Myra Tetteh, Senior Program Officer at the Blue Cross Blue Shield of Michigan Foundation. “It’s exciting to see results, and because of this program, so many individuals met their dental goals. We are proud to support a project with a community component as strong as this one.”
The researchers noted that significant access barriers related to cost cannot be solved by these peer-led interventions, so there’s more work to be done. But the progress thus far has meant a lot to them personally.
“This project has been very fulfilling,” Dr. Rulli said. “As an academician you do a lot of things, you do a lot of research and sometimes you have something that might be statistically significant but is it clinically significant? Is it relevant to real life? And in this case, I feel it is very much so.”
Dr. Lapidos added that more work can be done if health care integration can continue to be prioritized the way it was because of this Investigator Initiated Research Award.
“Something that the Blue Cross Blue Shield of Michigan Foundation has enabled us to do is to work interprofessionally toward making health care more integrated,” Dr. Lapidos said. “This funding has been of incredible value toward this interprofessional collaboration that is not always easy to do in our siloed systems of care. But we have a psychiatry department and a school of dentistry working together to benefit people of the community in partnership with a community advisory board, which would not have been possible without this funding.”
Read more Foundation stories:
- Arab American Dementia Outreach Program Helps Michigan’s Middle Eastern Community Shatter the Stigma Associated with Seeking Dementia Care
- Groundbreaking Rx Kids Cash Transfer Program in Flint Could Improve Health Outcomes for Generations of Children
- Michigan Surgical Quality Collaborative Teams with BCBSM Foundation to Improve Colorectal Cancer Surgery Outcomes Statewide
Photo credit: Dr. Lapidos/U of M's community partners





