Blue Cross Blue Shield of Michigan and Blue Care Network continued to respond to the COVID-19 pandemic in 2022 – providing $739 million in support to members for testing, treatment and vaccine administration. Like many organizations across the state and nation, Blue Cross mobilized resources in new ways to serve our members and customers. We also supported Michigan communities and partnered with doctors and hospitals to ensure access to health care and COVID-19 vaccines.
Here are some highlights of Blue Cross’ response to the crisis:
- Since the onset of the COVID-19 pandemic, Blue Cross has devoted $2.8 billion to support members, providers and employers. That includes $739 million in 2022 for COVID-19 testing, treatment and vaccination.
- Trusted advice to customers: Businesses needed information, insight and support from their health care partner. Blue Cross created a group customer command center and small group customer help line to quickly respond to customer questions.
- Support for community needs: In addition always being ready to help our members and customers, Blue Cross’ social mission is focused on improving the health of everyone in Michigan. For this reason, we continue to support community-based organizations to help address food insecurity for children and families, as well as organizations that help seniors and other vulnerable populations receive care and services.
- Partnerships with health care providers: We worked diligently to supply financial support early in the pandemic, reduce burdens and keep partner health care providers informed and connected. By helping stabilize normal cash flow, we worked to ensure providers were able to keep their doors open in a time of crisis.
In 2020, Blue Cross donated $1 million to be used for emergency personal protective equipment (PPE) kits for Michigan dentists, returned more than $21 million in one-time credits to more than 180,000 members with commercially insured individual health care plans and returned more than $100 million in credits to senior members, employer group customers and 2019 individual plan subscribers on their health, dental and vision premiums.
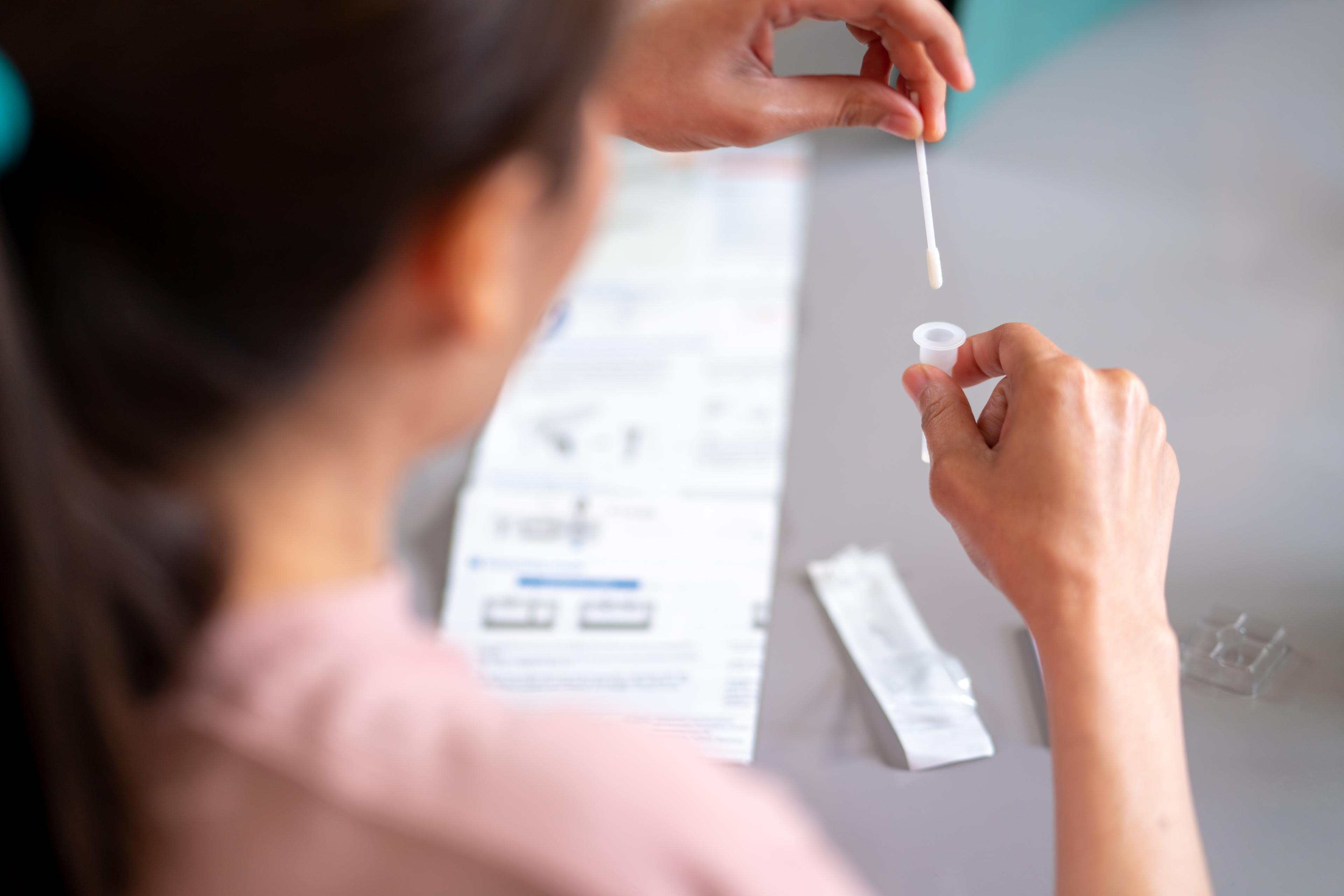
To ensure members could access needed care, during the onset of COVID-19 Blue Cross waived all member copays, deductibles and coinsurance for COVID-19 treatment (through Sept. 30, 2021) and testing.
Coverage for telehealth services was expanded when in-person visits were limited and limits on prescription refills were waived during certain periods to avoid shortages, along with many other member-focused efforts.
Photo credit: Robin Schwartz for Blue Cross Blue Shield of Michigan