Two projects within the cardiovascular collaborative improve patient safety by reducing opioids and reducing radiation exposure
Debbie Reinheimer
| 3 min read

Participants in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) have improved patient safety through two important projects. First, physicians have reduced the number of opioid pills prescribed to patients following certain vascular surgeries. Second, they reduced radiation exposure during angioplasty procedures.
In the first project, participating physicians saw the need and the opportunity to reduce the number of opioid pills prescribed after endovascular aneurysm repair and carotid endarterectomy procedures.
“Research showed more than 75 percent of patients took nine or fewer opioid pills after these procedures. Prescribing more pills than needed leaves excess pills circulating in the community and increases the chances that the pills will fall into the wrong hands,” said Peter Henke, M.D., director, BMC2 Vascular Surgery. “Fewer prescribed pills also means less of a chance for a patient to develop a dependency on them.”
Using recommendations from Michigan OPEN, BMC2 participants set a goal in 2019 that fewer than 10 opioid pills would be prescribed in 70 percent of cases. By the end of 2021, they had surpassed that goal, reaching nearly 90 percent of cases. The CQI, working in collaboration with the participants, has set a new goal to decrease post-procedure opioid prescriptions to just four pills.
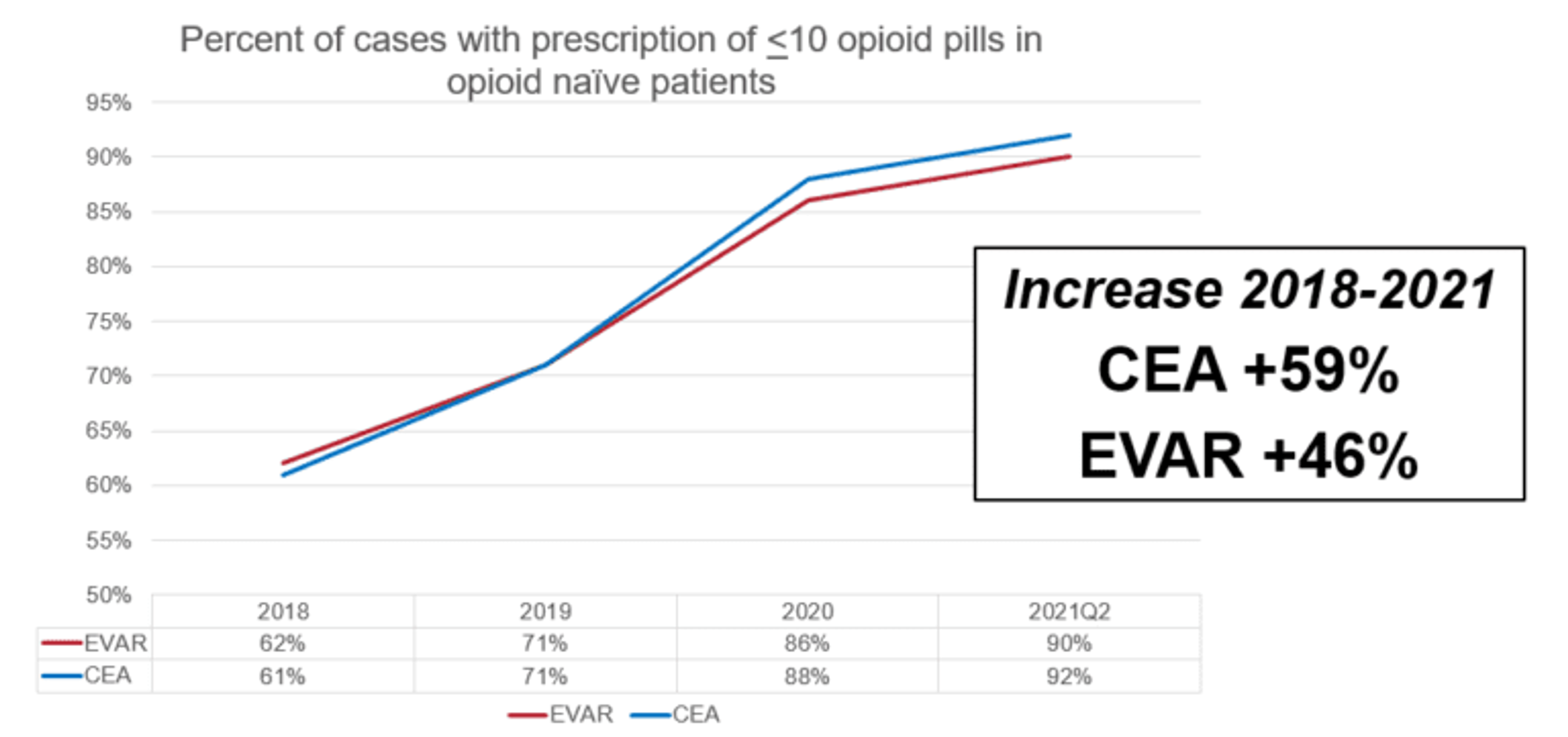
Source: BMC2
“We have found that most patients can control their pain levels with over-the-counter medication. By collecting and sharing data and best practices, physicians across the state have been able to quickly change their prescribing patterns and match pain control to their patients’ actual needs,” said Dr. Henke.
Radiation Reduction
In the second project, BMC2 participants reduced the amount of harmful radiation exposure to both patients and staff during percutaneous coronary intervention procedures (angioplasty and stenting.)
All PCI procedures need Xray radiation, but excessive radiation administered during PCI is associated with short-term tissue reactions and lifetime risk for developing cancer. The risk for negative outcomes increases if the radiation dose exceeds documented thresholds (5Gy). Patient radiation doses during PCI also put catheterization laboratory staff at risk from the effects of radiation.
So BMC2 participants developed best practices that include safety education, limiting fluoroscopy intensity and exposure time, and limiting cineangiography. Best practices to reduce physician and staff radiation dose include protective gear, increasing distance from patient and shielding.
The goal was to reduce the percent of cases with high level (>5 Gy) radiation doses to below 2 percent per hospital per year. Participants were given statewide radiation-related data which were discussed at consortium-wide meetings. BMC2 hosted a radiation-safety education webinar and posted it to their YouTube channel for broader dissemination.
BMC2 participating hospitals surpassed the goal and achieved an overall 43-percent decrease in cases with high dose (>5 Gy) radiation exposure, preventing negative short- and long-term consequences in hundreds of patients and catheter lab staff members every year.
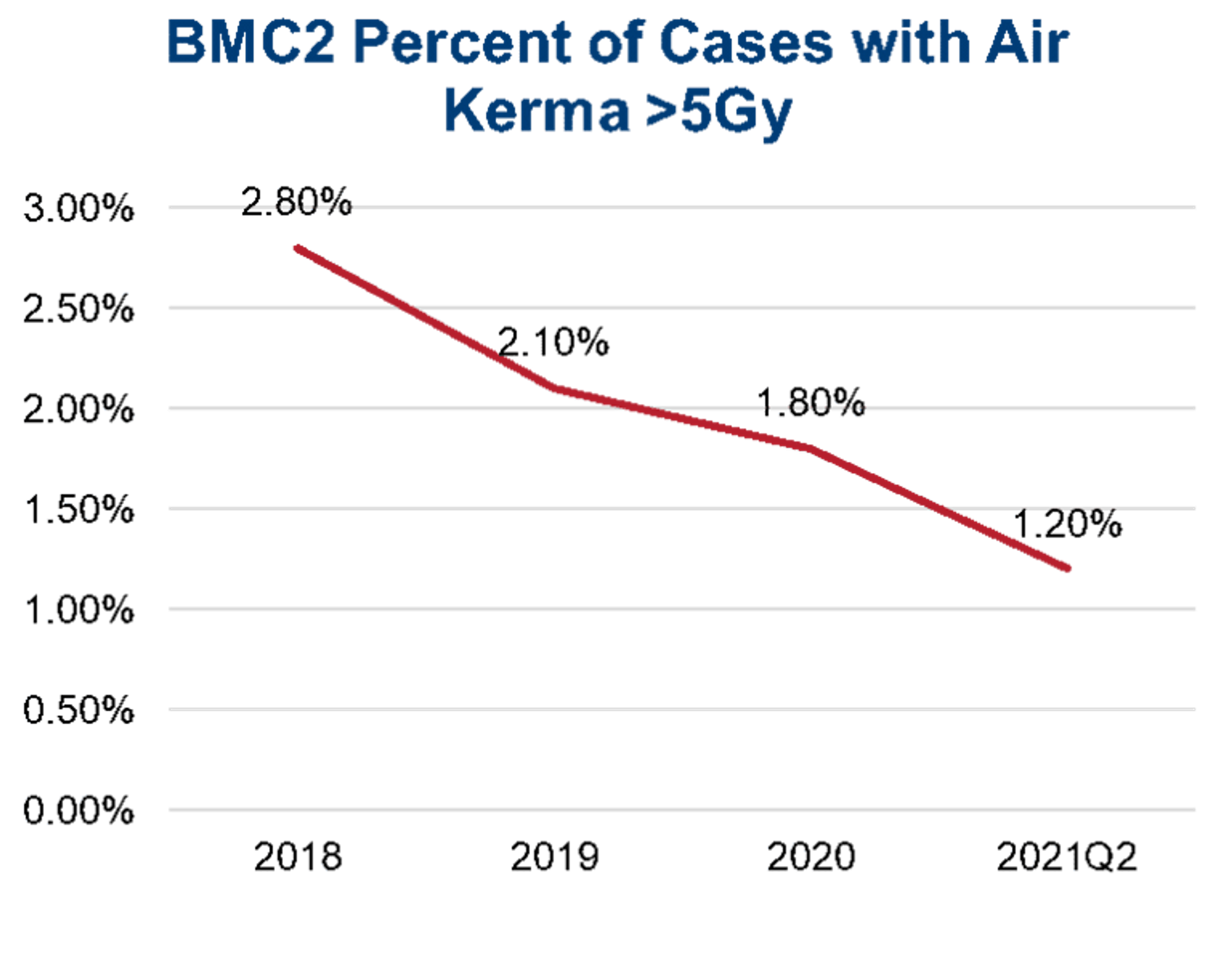
Source: BMC2
“It is encouraging to see the progress BMC2 has made with respect to improving radiation safety in catheterization labs across Michigan. In addition to decreasing patient radiation doses, the efforts of BMC2 have likely improved occupational safety in catheterization labs since lower patient radiation doses should result in lower radiation exposure for physicians and staff,” says Ryan Madder, M.D., medical director of the Catheterization Lab and section chief of Interventional Cardiology at Spectrum Health, and strategic advisor to BMC2.
“One of the merits of the collaborative quality initiatives, like BMC2, lies in the cooperative framework that encourages sharing of data and best practices to benefit everyone. With participants from across the state working together on shared clinical quality and patient safety goals, the competitive barrier is mitigated. Physicians learn from their peers and can quickly change practice patterns to make rapid improvements,” said Faris Ahmad, M.D., medical director, Blue Cross Blue Shield of Michigan.





